By: Evelyn Lirri
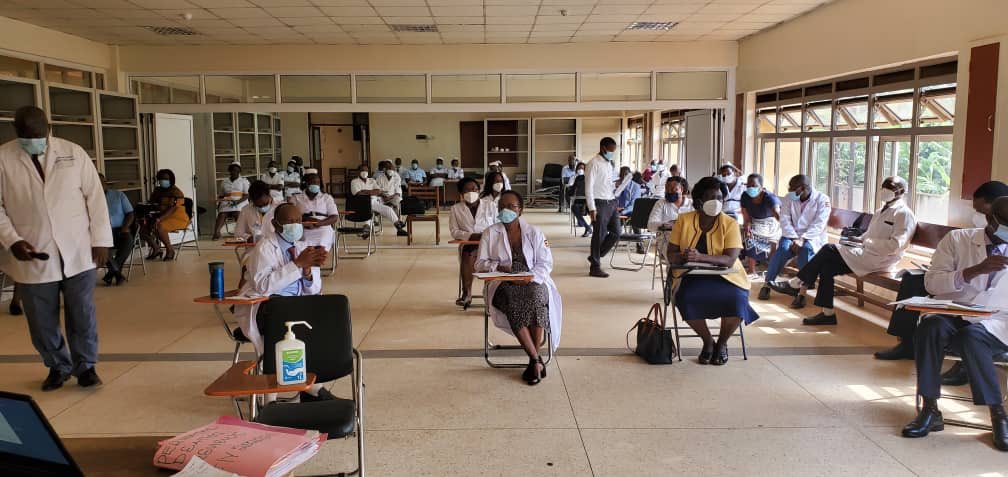
As COVID-19 cases continue to rise in Uganda, concern about how the health care system should go about addressing this threat is also growing.
Experts are now rethinking what the best strategy could be to control the spread, while managing those who have been infected without overwhelming health facilities.
At the forefront of these discussions is whether for instance, the government should continue hospitalizing everyone who tests positive for COVID-19, especially individuals who may only present mild symptoms or no symptoms at all. The other emerging school of thought is to encourage self-isolation at home. The proponents are urging government to have health workers effectively follow up patients to ensure they are recovering well and following the Standard Operating Procedures (SOPs) including social distancing and wearing masks at all times to minimize any risk of infection.
Part of the country’s COVID-19 control strategy has focused on ensuring that every individual who tests positive is isolated and managed within a hospital setting. The admission duration has been 18 days. In this period, it is expected that with treatment, patients should be able to show no further symptoms of the virus. A second confirmatory test is then usually conducted before those who test negative are discharged. Rising numbers amidst limited resources in terms of hospital capacity across the country renders such a comprehensive approach, although the most ideal and desirable, rather a luxury. It was tenable when the country had a handful of cases. With cases now in the region of thousands, tough times are calling for tough measures.
The Ministry of Health now says it will start discharging individuals who test negative after 10 to 12 days from the onset of symptoms, instead of the 18 days. This is also in line with global recommendations that had already been issued by the Centres for Disease Control and Prevention (CDC). According to CDC, it is estimated that a person who has had COVID-19 stops being contagious 10 days after symptom onset and after at least three days without a fever. Such a person can then be released from isolation.
“If a person with COVID-19 is treated, we see they are testing negative for the virus after 10 days. Which means there should be no need to keep them in the hospital beyond that duration of time,” says Dr. William Worodria, the health ministry’s COVID-19 case manager.
He explains that most of the cases of the coronavirus that the country has registered have been mild, which has subsequently contributed to high numbers of recoveries. According to Dr. Worodria, less than 20 per cent of people confirmed with COVID-19 in the country have had moderate to severe forms of the disease, with a big percentage presenting with mild forms and few symptoms or no symptoms at all—what is known as asymptomatic COVID-19 cases.
Research has shown that people become infectious before they start feeling sick, which has been one of the biggest contributors to the spread of the disease, and also explains why globally, it has been difficult to contain.
Data from the Ministry of Health shows confirmed cumulative COVID-19 cases stand at about 3,300, with slightly over 1,500 recoveries registered (by September 4.)
One of the reasons for the change of hospitalization days is the costs involved. Keeping people longer in hospitals means more spending for the government, which in the long run becomes unsustainable especially in the face of rising infections.
Currently, it costs about Shs150,000 per day to keep one case of COVID-19 in hospital, according to Dr. Mukuzi Muhereza, the Secretary General of the Uganda Medical Association (UMA).

Reducing the hospital admission days, he says, is a good move by the government, which will also help free up money for the health care system. Besides the financial cost, Dr. Muhereza says health workers will also have the time to concentrate on individuals with moderate to more severe forms of the disease.
Since most people who have so far tested positive for COVID-19 in Uganda have a mild form of the disease, Dr. Muhereza suggests that many could be encouraged to isolate at home as long as they are able to follow Ministry of Health guidelines.
Experts have been making the case that some of the hospitalization for COVID-19 is unnecessary because as infections continue to spread, more people who test positive for the virus will require hospitalization, which in the long run overwhelms the entire health system, if every mild case is admitted and has to wait more than 10 days before being discharged.
The experts suggest that only individuals with moderate to severe forms of the disease should be hospitalized.
The President has previously noted that the country has capacity to deal with the COVID-19 pandemic should the number of people requiring hospitalization rise, including turning the Mandela National Stadium into a 40,000-bed field hospital.
Dr. Frank Asiimwe of the Uganda Medical Association recently wrote about some of the things that the Ministry of Health could focus on as it manages the new wave of infections, on top of stopping to admit every individual who tests positive.
As soon as a COVID-19 case admitted to the hospital becomes asymptomatic, Dr. Asiimwe argues, “discharge them to continue care from home. Don’t wait for them to test negative first.”
Playing with fire?
In countries where self-isolation can work effectively, people who test positive for the virus with mild symptoms have often been encouraged to self-isolate in their homes for 14 days.
Countries such as Kenya are already implementing the home-based care approach.
And while this approach has indeed helped countries focus mostly on severe cases that end up in health facilities, implementing the same strategy in countries such as Uganda will come with major challenges.
For instance, Dr. Muhereza points out that it may be difficult to implement home based isolation effectively for the majority of the population especially in urban centres owing to the living conditions in most households.
“Given how people live in most households, this is not something that will be easy to implement. Also, how do you ensure that people remain home for the mandated period of time?” he asked.
One of the protocols for home-based isolation from the World Health Organisation is that a separate ventilated bedroom should be available to a COVID-19 patient so that they can isolate and reduce their risk of spreading the virus.
In some ways though, the ministry is starting to take this recommendation. Some people who have tested positive for COVID-19 within Kampala, Wakiso and Mukono have been advised to self-isolate at home. But not so much because the health ministry hopes to promote home self-isolation for now, but because as the Health Minister Dr Jane Ruth Aceng noted, health workers have not been able to easily trace the homes of some of the positive cases on time to evacuate them to health facilities. The plan, the ministry says, is still to have them treated from a health facility.

Most people, especially in the urban areas live in crowded dwellings where social distancing has been difficult to implement, and where people are also not taking personal responsibility to wear face masks and social distance.
This failure to follow basic precautions is what is driving a rapid spread of COVID-19 infections since lockdown measures were eased in June, according to Dr Monica Musenero, the presidential advisor on epidemics.
“We are having a rapid spread of the virus because the public has not held up to their end of the bargain. People are not social distancing, washing hands with water and soap or wearing masks,” she says.
She explains that while Uganda started on a good trajectory, several factors, including the current political environment—where politicians are occasionally holding rallies without observing preventive measures is contributing to the challenge at hand. But she is optimistic the curve can still be flattened.
“We still have a chance to save ourselves. If people wash their hands, wear a mask and social distance, then we will be able to manage the disease. Infections will be there but the number of people in hospitals will be fewer,” says Dr. Musenero.